Herniated and Bulging Discs
the difference between a bulging disk and a herniated disk?
Disks act as cushions between the vertebrae in your spine. They're composed of an outer layer of tough cartilage that surrounds softer cartilage in the center. It may help to think of them as miniature jelly doughnuts, exactly the right size to fit between your vertebrae.
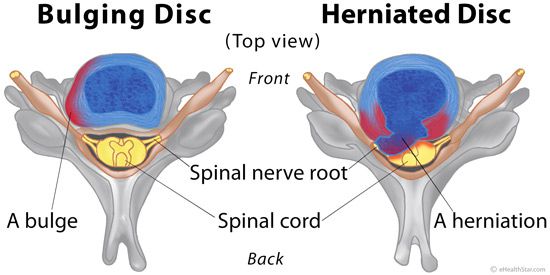
Disks show signs of wear and tear with age. Over time, disks dehydrate and their cartilage stiffens. These changes can cause the outer layer of the disk to bulge out fairly evenly all the way around its circumference — so it looks a little like a hamburger that's too big for its bun.
A bulging disk doesn't always affect the entire perimeter of a disk, but at least a quarter if not half of the disk's circumference is usually affected. Only the outer layer of tough cartilage is involved.
A herniated disk, on the other hand, results when a crack in the tough outer layer of cartilage allows some of the softer inner cartilage to protrude out of the disk. Herniated disks are also called ruptured disks or slipped disks, although the whole disk does not rupture or slip. Only the small area of the crack is affected.
Compared with a bulging disk, a herniated disk is more likely to cause pain because it generally protrudes farther and is more likely to irritate nerve roots. The irritation can be from compression of the nerve or, much more commonly, the herniation causes a painful inflammation of the nerve root.
If an imaging test indicates that you have a herniated disk, that disk might not be the cause of your back pain. Many people have MRI evidence of herniated disks and have no back pain at all.
You may have heard the term "slipped disc" used to describe a low back injury. Discs do not actually "slip". Rather, they may herniate or bulge out from between the bones. A herniation is a displaced fragment of the center part or nucleus of the disc that is pushed through a tear in the outer layer or annulus of the disc. Pain results when irritating substances are released from this tear and also if the fragment touches or compresses a nearby nerve. Disc herniation has some similarities to degenerative disc disease and discs that herniate are often in an early stage of degeneration. Herniated discs are common in the low back or lumbar spine.
What causes discs to herniate?
Many factors decrease the strength and resiliency of the disc and increase the risk of disc herniation. Life style choices such as smoking, lack of regular exercise, and inadequate nutrition contribute to poor disc health. Poor posture, daily wear and tear, injury or trauma, and incorrect lifting or twisting further stress the disc. If the disc is already weakened, it may herniate with a single movement or strain such as coughing or bending to pick up a pencil.
How do I know if I have a disc herniation?
Herniated discs are most likely to affect people between the ages of 30 and 40. Disc herniations may be present without causing pain. The most common symptom will be pain in the area of the herniation that may radiate across the hips or into the buttocks. You may also experience numbness or pain radiating down your leg to the ankle or foot. If the herniation is large enough, you may notice weakness with extension of your big toe and you may be unable to walk on your toes or heels. In severe cases of lumbar disc herniation, you may experience changes in your bowel or bladder function and may have difficulty with sexual function.
How is a disc herniation treated?
Mild to moderate disc herniations can usually be treated conservatively with stretching, exercise therapy and chiropractic care. More advanced cases will often require some form of spinal decompression, such as traction or mechanical decompression, in conjuction with chiropractic care.
Occasionally, a herniation may be severe enough to warrant surgical intervention. These cases are usually reserved as a last resort when other forms of therapy have failed to relieve pain, or if there is significant compression of the spinal cord or nerves.